- Research
- Open access
- Published:
Perceptions of adults with type 1 diabetes toward diabetes-specific quality of life measures: a survey-based qualitative exploration
Health and Quality of Life Outcomes volume 22, Article number: 70 (2024)
Abstract
Background
Diabetes-specific quality of life (QoL) questionnaires are commonly used to assess the impact of diabetes and its management on an individual’s quality of life. While several valid and reliable measures of diabetes-specific QoL exist, there is no consensus on which to use and in what setting. Furthermore, there is limited evidence of their acceptability to people with diabetes. Our aim was to explore perceptions of adults with type 1 diabetes (T1D) toward five diabetes-specific QoL measures.
Methods
Adults (aged 18 + years) with T1D living in Australia or the United Kingdom (UK) were eligible to take part in ‘YourSAY: QoL’, an online cross-sectional survey. Recruitment involved study promotion on diabetes-related websites and social media, as well as direct invitation of people with T1D via a hospital client list (UK only). In random order, participants completed five diabetes-specific QoL measures: Audit of Diabetes-Dependent Quality of Life (ADDQoL-19); Diabetes Care Profile: Social and Personal Factors subscale (DCP); DAWN Impact of Diabetes Profile (DIDP); Diabetes-Specific Quality of Life Scale: Burden Subscale (DSQoLS); Diabetes Quality of Life Questionnaire (Diabetes QOL-Q). They were invited to provide feedback on each questionnaire in the form of a brief free-text response. Responses were analysed using inductive, thematic template analysis.
Results
Of the N = 1,946 adults with T1D who completed the survey, 20% (UK: n = 216, Australia: n = 168) provided qualitative responses about ≥ 1 measure. All measures received both positive and negative feedback, across four themes: (1) clarity and ease of completion, e.g., difficulty isolating impact of diabetes, dislike of hypothetical questions, and preference for ‘not applicable’ response options; (2) relevance and comprehensiveness, e.g., inclusion of a wide range of aspects of life to improve personal relevance; (3) length and repetition, e.g., length to be balanced against respondent burden; (4) framing and tone, e.g., preference for respectful language and avoidance of extremes.
Conclusions
These findings suggest opportunities to improve the relevance and acceptability of existing diabetes-specific QoL measures, and offer considerations for developing new measures, which need to be better informed by the preferences of people living with diabetes.
Background
Diabetes-specific quality of life (QoL) refers to an individual’s perception of the impact of diabetes on their QoL, or how diabetes affects aspects of life important to them [1, 2]. Several diabetes-specific QoL assessment tools exist [2,3,4,5], with no consensus on which to use and in what setting. Likely relatedly, there has also been a lack of systematic QoL assessment (diabetes-specific or generic) in diabetes research and clinical practice [1]. In response, practical guidance and frameworks have been proposed to support appropriate diabetes-specific QoL questionnaire selection [1, 3, 6], including consideration of questionnaire aims, intended population, rigour of development process, psychometric properties, sensitivity to change, participant burden, content face validity, and acceptability among the intended audience. While considerable evidence for the psychometric properties of established diabetes-specific QoL questionnaires (across populations and linguistic translations) exists, responder perceptions toward, and acceptability of, questionnaire’s remains limited [3, 4, 7].
Involvement of the intended group in questionnaire design and refinement is considered a methodological necessity to assure content validity and acceptability [8,9,10,11]. However, the extent to which people with diabetes have traditionally been consulted in the development of diabetes-specific QoL measures varies (see Table 1), and few subsequent studies have examined respondent perceptions to inform questionnaire refinement or selection [7, 12, 13]. While some more recently developed questionnaires have involved such community involvement and piloting [14], questionnaires developed decades ago continue to be used most widely and whether they remain fit for purpose or are acceptable to contemporary study participants warrants consideration. Researchers and clinicians must rely on the typically sparse details reported within in scale development and psychometric testing publications, with questionnaire acceptability often indicated by response rate rather the respondent perceptions.
Previously, we reported quantitative findings of the ‘Your Self-management And You: Quality of Life’ (YourSAY: QoL) study, which was the first ‘head-to-head’ comparison of the psychometric properties and acceptability of five questionnaires designed to assess diabetes-specific QoL among adults with type 1 diabetes (T1D) living in Australia and the United Kingdom (UK) [7]. The findings suggested largely positive and consistent acceptability user ratings across the diabetes-specific QoL measures, as quantitatively derived by five study-specific single-items on a 5-point Likert scale. However, these published data provide no insights into the specific reasons for the largely positive views, nor explanation for respondents’ negative ratings. In addition to the user ratings, survey participants were invited to provide brief qualitative feedback. In combination with published development processes and psychometric evaluation, the preferences of people with T1D can inform recommendations for the selection of diabetes-specific QoL tools as well as the improvement of existing and novel questionnaires can be made.
Therefore, the current study explores the qualitative feedback collected in the YourSAY: QoL survey to understand what adults with T1D in Australia and the UK like and dislike about five contemporary and/or commonly used diabetes-specific QoL measures.
Methods
The YourSAY: QoL study was a cross-sectional survey administered online, using a pragmatic mixed-methods approach to explore questionnaire acceptability. Study methods have been described in detail elsewhere, and are included below [7]. For this substudy, a descriptive theoretical framework was employed with the aim of providing a comprehensive summary of participant questionnaire perceptions and preferences. This approach is well-suited to ‘thin’ data collected via survey free-text responses.
Participants and recruitment
Eligible participants for the overall survey were adults (aged 18 + years) with a self-reported diagnosis of T1D or type 2 diabetes (T2D), living in either Australia or the UK. Participants were recruited using convenience sampling through websites, e-newsletters/blogs and social media (Twitter, Facebook). In the UK only, a social media advertising company was contracted to promote study advertisements using Facebook, and 1,921 consenting adults with T1D under the care of Sheffield Teaching Hospitals NHS Trust were invited to take part (via letter or email). Potential participants were directed to an online survey hosted via Qualtrics™ (a secure online survey platform). Following informed consent and eligibility screening, eligible participants were directed to the survey proper.
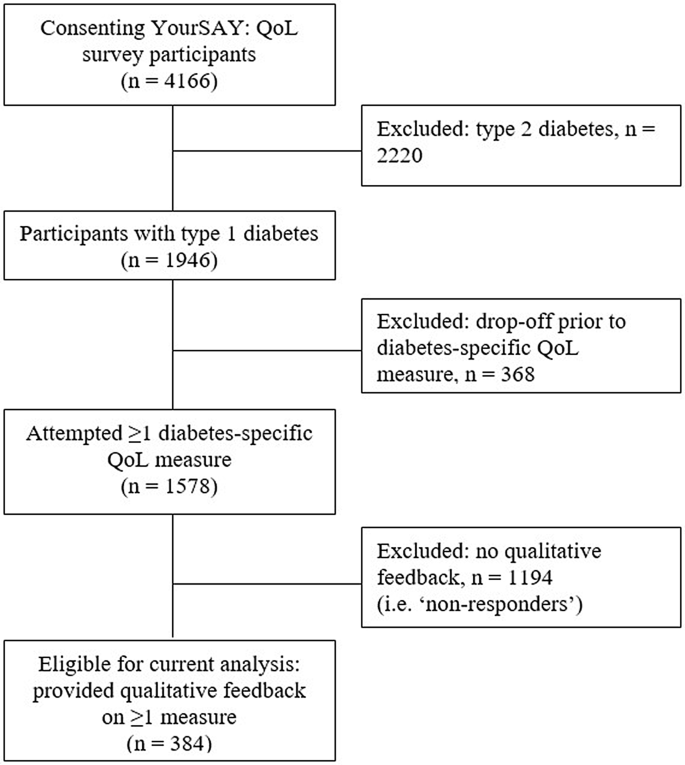
The YourSAY: QoL survey was completed by N = 4166 participants (T1D: n = 1946, 47%). Inclusion criteria for the current analysis were self-reported T1D, and provision of qualitative feedback on at least one attempted diabetes-specific QoL questionnaires. Participant flow and reasons for exclusion are detailed in Fig. 1. The current qualitative study reports on a subsample of n = 384 YourSAY: QoL participants.
Measures
Participants were invited to complete five diabetes-specific QoL measures (detailed in Table 1).The questionnaire selection process and psychometric analyses are reported elsewhere [7]. The five Diabetes-specific QoL measures were presented in random order to control for order effects, and optimise complete data per questionnaire in the case of early drop off. Following each questionnaire, participants were presented with five study-specific questions in which they were asked to rate ( 5-point scale: 1 = strongly disagree to 5 = strongly agree), the clarity, relevance, ease of completion, length, and comprehensiveness of the questionnaire (reported elsewhere) [7]. Participants were then asked the following free-text qualitative question: “Your feedback is important to us. Please feel free to comment below on anything you particularly liked or disliked about this questionnaire”.
Demographic (age, sex, location of residence, primary language) and self-reported clinical data (diabetes duration, primary treatment, number of diabetes-related complications) were also collected.
Data handling and analysis
Descriptive statistics for key demographic and clinical characteristics and differences between ‘responders’ (eligible final sample) and non-responders (participants with T1D who attempted ≥ 1 measure but provided no qualitative feedback) were calculated (IBM SPSS Statistics). Between group differences were assessed via Student’s t-tests for continuous variables and Pearson’s Chi-Square for categorical data.
Qualitative data were screened for invalid responses (e.g. “N/A”, “nil”) and uploaded to QSR NVivo for thematic template analysis, applying an inductive (data-driven) approach [22]. In template analysis, a coding template (which summarises the (sub)themes in a meaningful order) is developed, refined and applied iteratively to the data. This approach is well-suited to vast but shallow survey data collection, as template analysis does not require distinction between descriptive and interpretive themes. Following familiarisation with the data, J.Sc proposed an initial coding template, which was iteratively reviewed and refined following coding application by JSc and E.H-T, as well as discussion with J.Sp. Minimal coding disagreement was identified, discussed and resolved between authors. The final framework was applied to the remaining responses by J.Sc. Names and descriptions of the final themes and subthemes were agreed among all authors, and example quotes reviewed to ensure they represented the data adequately and reflected the study aims.
J.Sc, an undergraduate researcher at the time of analysis, led qualitative data analysis, reflecting on data initially without pre-conceived assumptions about measures, and discussing findings with the remaining authors (expertise: health psychology, health services, clinical diabetes) who drew on their deep understanding [1, 2], and prior application of the assessed tools (including contributions to their development [21], refinement, [18] or English translation [20]) in their interpretation of findings. Representation of both positive and negative feedback for each measure was prioritised to challenge any predefined ideas about preferred measures.
Results
Characteristics of the eligible sample (respondents, n = 384), and those who attempted the diabetes-specific QoL questionnaires but did not provide qualitative feedback (non-respondents, n = 1194), are shown in Table 2.
Most respondents attempted all five diabetes-specific QoL measures of interest (n = 344, 90%) and provided qualitative feedback on one questionnaire (n = 220, 57%), most commonly for the DSQoLS (see Table 3). Across the five measures, a total of 711 qualitative responses were provided. A minority of participant feedback included general comments (e.g. all five questionnaires were perceived by some as “good”, “fine”, “liked”, or described as “enjoyable” and “interesting”) with no further detail. Specific feedback was organised within four main themes: (1) clarity and ease of completion; (2) relevance and comprehensiveness; (3) length and repetition, and (4) preferences and impact of questionnaire wording and tone. Overall themes and sub-themes are described below, and quotes relevant to the five questionnaires are shown in Table 3.
Questionnaire clarity and ease of completion
In addition to general endorsements that questionnaires are “simple”, “easy”, and “straightforward”, participants provided specific feedback relating to the clarity of instructions and questionnaire wording; suitability of response options, and difficulty isolating the impact of diabetes on QoL.
Instructions and question wording
Differing views were offered about whether questionnaire instructions or questions were clear and easy to understand, as well as preferred questionnaire attributes. For instance, some participants praised the inclusion of examples in the Diabetes QOL-Q (‘I can go out or socialise as I would like, e.g., cinema, concerts…’), suggesting that it helped to clarify what is being asked, while another participant reported the inclusion of such examples as “patronising”.
Consistently, respondents indicated that the if/then wording used in the ADDQoL-19 was “confusing” and questions containing double negatives (i.e. item 17: “If I did not have diabetes, I would have to depend on others when I do not want to”) were “illogical” and “incomprehensible”. They also indicated that the broad question wording that encompassed diverse situations made it difficult to answer the questions. For example, item 3 of the DIDP incorporates three separate concepts (i.e. ‘relationship with your family, friends and peers’) and item 8 of the ADDQoL-19 combines current experience of or wish for a ‘close personal relationship’ within a single question. Participants also found overly-specific wording did not capture their actual experience. For example, two DCP items assess the impact of diabetes on food intake, but not “when I would like” to eat. One respondent provided feedback on the seventh item of the modified DIDP (‘Your freedom to eat as you wish’), reporting that this question stood out and was “much more specific than the other[s]”.
For the DCP and DSQoLS, participants also indicated that the timeframe referred to in the instructions (e.g. “in the past 4 weeks”, “in the past year”) was confusing, “easily forgotten”, or “too long”.
Response options
There was mixed feedback regarding the preferred number of response options and phrasing. Some participants reported liking the bi-directional response scale used in the DIDP, while others stated that they found it confusing or that it did not account for the potential combined positive and negative impacts of diabetes on particular aspects of life, such as physical health. In general, participants favoured inclusion of a “not applicable” response option, and some reported that this option was missing from the DCP and DSQoLS. Across measures, several participants indicated a desire to explain the underlying reasons for their response and participants positively reviewed the inclusion of an open-ended question inviting a free-text response in the ADDQoL-19.
Difficulty assessing the impact of diabetes
In rating the impact of diabetes on a particular aspect of life, the ADDQoL-19 asks participants to imagine their life without diabetes (e.g. ‘If I did not have diabetes, my quality of life would be…’). Though some participants reported that the opportunity to reflect on their life without diabetes was “an interesting concept”, others disliked this hypothetical phrasing and found the questions “impossible” to answer. While the other four measures of interest do not instruct participants to compare or rate their QoL against a life without diabetes, some participants reported difficultly responding as it’s “the only life I know” and that they may have over- or underestimated the impact of diabetes on their QoL. Participants also reported difficulty isolating diabetes from the impact of other life factors (e.g., other health condition, responsibilities, financial challenges). Some indicated a preference for a generic measure, which would allow participants to rate their QoL overall.
Questionnaire comprehensiveness and relevance
Where participants reported questionnaires as irrelevant, some indicated an inability to identify with the questionnaire, or that the questionnaire assumed a view of diabetes that did not reflect (their) reality. The lengthy DSQoLS (57 items) had the most references discussing perceptions of its (ir)relevance, while feedback on the shorter DIDP (7 items) indicated that it was “simplistic”.
Relevance of specific aspects of life and perceived omissions
Conflicting feedback was identified regarding the relevance of measured domains, particularly related to the impact of diabetes on finances. More typically, UK participants perceived such questions as irrelevant and suggested their removal, while Australian respondents endorsed such questions as relevant. Other specific questionnaire items reported as relevant included future health and development of diabetes complications (DSQoLS); emotional well-being (DIDP and DSQoLS, ); body image and family relationships (Diabetes QOL-Q). In contrast, irrelevant items commonly related to romantic partners and intimacy (DSQoLS, ADDQoL-19); driving (Diabetes QOL-Q); eating as you wish (ADDQoL-19); treatment modality-specific questions (DSQoLS), and experience of hypoglycaemia (DSQoLS).
Table 4 lists topics, or aspects of life, which participants perceived as missing from a questionnaire or not adequately assessed. Across questionnaires, commonly perceived omissions related to the impact of diabetes on mental / emotional health, and on finances, as well as the impact of diabetes management activities (e.g. insulin administration modality; diet; glucose monitoring) and extreme glucose levels on overall QoL. The Diabetes QOL-Q had the fewest references to omissions overall (n = 22), while the DSQoLS had the most reported omissions (n = 69), of which most referred to the impact of hyperglycaemia.
Questionnaire length and repetition
Related to, but discrete from comprehensiveness, participants commented on the length of measures, and were divided in their preference for brevity versus breadth. For example, the 7-item DIDP was described both as “brief and direct” and “so brief it was almost offensive”. Similarly, the 57-item DSQoLS was reported by some to be “too long” and by others as allowing for a detailed or comprehensive assessment (Theme 2). Item repetition was reported for the DSQoLS, to a lesser degree for the DCP and Diabetes QOL-Q and not at all for the ADDQoL-19 or the DIDP. Participants reported that repetitive questioning was “depressing”, overstated the relevance of certain topics/life aspects (i.e. the 11 DSQoLS items examining the impact of hypoglycaemia), and left them feeling more “worried”.
Questionnaire framing
Some respondents reported disliking the negative framing used by the ADDQoL-19, DCP and DSQoLS because they perceived it as placing a focus on the limitations of diabetes. In contrast, others appreciated the ADDQoL-19’s recognition of the “negative aspects of life”. Feedback about the positively-framed Diabetes QOL-Q was similarly divided between those who liked the “more positive manner” and those who felt it painted a “falsely positive picture”. Participants also reflected on the specific words and phrases used, reporting that certain terms (e.g. ‘normal’ and ‘control’ in the Diabetes QOoL-Q; ‘burden’, ‘worry’, ‘bother’ in the DSQoLS) made them feel like a “victim” or implied that diabetes controlled them. In contrast, the language used in the ADDQoL-19 was described as “extremely respectful”.
Discussion
Consistent with quantitative user rating assessment [7], study findings suggest that there is no unequivocally favoured diabetes-specific QoL measure among adults with T1D from Australia and the UK. However, an acceptable measure needs to be easy to understand and complete; comprehensive and personally relevant; brief, without repetition; neither overly negative/nor positive; and adopting respectful language. Review of the questionnaires’ attributes (Table 1) suggests greatest alignment to reported preferences for the ADDQoL-19, DIDP, and Diabetes QOoL-Q (i.e. fewer reported omissions, greater perceived relevance, opportunity for personalisation, no/low repetition of domains, and/or neutrally worded). These three measures were also previously identified as having strongest psychometric performance among YourSAY: QOL participants with T1D [7]. Consideration and application of respondents’ preferences in the review of existing measures, or the development of new questionnaires, may further improve acceptability, respondent experience and data quality for future studies.
Careful consideration of questionnaire wording is needed to minimise cognitive load and improve acceptability [23]. For example, the ADDQoL-19 has been criticized for its unique use of hypothetical questioning [2, 24], which is presumed to be cognitively demanding [24, 25], and is not recommended [9]. While ADDQoL-19 developers suggest that such questioning results in a more realistic assessment of the impact of diabetes [26], the differential basis for hypothetical responses (e.g. some may recall a time pre-diabetes, others may draw on social comparisons) may impact data reliability. Interestingly, difficulty assessing the specific impact of diabetes due to a lack of comparison (i.e. life without diabetes) or inability to isolate its impacts (i.e. from other health conditions or life factors) was not unique to the ADDQoL-19, but reported across all measures. Relatedly, a preference for a more holistic measure of health-related or general QoL (e.g. the new EQ-HWB) [27] was reported by some participants, while for others, diabetes-specific questionnaires enabled a unique opportunity for reflection and acknowledgment of the challenges of diabetes. Further qualitative research might examine individual differences in how respondents interpret and complete condition-specific questionnaires.
Some participants reported difficultly completing questions that included double-barreled concepts (e.g. DIDP item: ‘your relationship with your family, friends and peers’) or were too broad (e.g. DIDP item: ‘your physical health’). Their separation into distinct items may be considered, though this has implications for scale brevity and could place too much emphasis on specific domains (as was reported for the DSQoLS regarding hypoglycaemia and emotional burden). Regardless, omission of important QoL domains was not more commonly reported for the brief DIDP (which higher-order type wording) and good concurrent validity between DIDP total scores and longer measures has been established [7]. Thus, the DIDP may be appropriate where the intention is to measure the overall impact of diabetes on QoL, and/or identify global domains for further assessment or clinical discussion. Regardless of item specificity, or consistency with theorised domains of diabetes-specific QoL [28], none of the examined measures in the current study were without perceived omissions of important life aspects (domains).
Determinants of QoL are subjective and, accordingly, it is argued that QoL assessment should be tailored to the aspects of life deemed most important to a given individual [29]. For example, several participants commented on the irrelevance of finances, while others expressly reported the importance or omission of this domain. The inclusion and rating of irrelevant or unimportant QoL domains, and the exclusion of other relevant domains, may reduce meaningful scoring and/or lead to misguided intervention. However, few QoL questionnaires allow for such personalised assessment [30]. In an effort to personalise QoL within a standardised approach, the ADDQoL-19 employs average weighted impact scores incorporating perceived domain importance within scoring, and three measures allow for non-applicable responses to all (DIDP, Diabetes QOL-Q) or certain (ADDQoL-19) domains, which was viewed favourably by participants. Though applicability is not synonymous with importance. The collection of qualitative data in companion with quantitatively assessed QoL might help bridge the divide between personalised and standardized assessment [31]. Participants reported appreciation of the ADDQoL-19 free-text question, and across other measures reported a desire to elaborate on their responses. Regardless of the measure selected, inclusion of a free-text question might be considered for the mutual benefit of examining survey acceptability, increasing insights into the experience of diabetes, and/or identifying areas for clinical discussion. It is important that ethical consideration is given to the intended use of such data, and its collection is justifiable.
Interestingly, negative feedback suggesting scale irrelevance, and omission of important life aspects more typically related to the considerably longer DSQoLS, which does not allow for ‘not applicable’ responses and is the only evaluated measure intended only for use among adults with T1D (i.e. not also for use in T2D). At previously noted [7], the DSQOLS item profile is dissimilar to other questionnaires assessed, with inclusion of items relating to diabetes management, symptoms, fear of hypoglycaemia, and emotional burden. In contrast, the ADDQoL-19, DIDP and Diabetes QOL-Q assess the impact of diabetes on more global aspects of life, which may be consistent across diabetes types, treatments and experiences. However, the current findings cannot speak to the perceptions of, nor preferred measure attributes among those with T2D. It is possible that planned future inspection of the acceptability and psychometric performance of relevant questionnaires among participants with T2D may highlight differential preferences and scale performance, suggesting the need for tailored questionnaire selection, revision, or development by diabetes type (as has been a recent focus in the assessment of diabetes distress [32, 33]).
The overall strengths and limitations of the YourSAY: QoL study are detailed elsewhere [7]. A key strength of the current qualitative study is the survey method, which permitted feedback from a large sample, extending on prior quantitative exploration of questionnaire acceptability [7] and qualitative methods used to inform questionnaire development and/or debriefing. However, the inability to follow up participants and invite additional information is a limitation of the current approach. Further, a minority of participants provided qualitative feedback (likely due in part to the burdensome overall survey length which resulted in substantial participant attrition) and this group were found to be more highly educated and engaged and slightly less negatively impacted by diabetes, compared to the broader sample. Thus, this study does not address the prior gaps of biased samples when developing or validating measures, and further acceptability assessment is warranted to explore questionnaire perceptions among diverse subgroups (e.g. those with ethnically diverse background, low English proficiency and/or (health) literacy). Future questionnaire adaptations and design should be informed by, and tested within, the intended population prior to use. Finally, other potentially relevant measures have been excluded from the current study, such as those published in a language other than English and/or novel questionnaires developed and validated since conducting the study. Future research might employ the methods designed here or draw on the identified subthemes to evaluate the acceptability of other measures and / or within populations not incorporated in the current study.
Conclusion
This novel large-scale qualitative study identified user perceptions, and preferred measurement attributes, of five diabetes-specific QoL measures among adults with T1D. Study findings complement our previous psychometric ‘head-to-head’ comparison [7], and identified the ADDQoL-19, DIDP and Diabetes QOL-Q as more typically incorporating preferred questionnaire attributes. These data, in combination with published development processes and psychometric evaluation, may be used to inform future questionnaire selection as well as best-placed resourcing for the improvement of existing and development novel diabetes-specific QoL measures. For example, findings from the current study directly informed assessment of diabetes-specific QoL within the DAFNEplus (Dose Adjustment For Normal Eating) cluster randomised controlled trial [34]. Specifically, the ADDQoL was selected as the primary psychosocial outcome measure, reflecting scale acceptability, psychometric performance, as well as existing evidence for scale responsiveness to intervention (including DAFNE [35]). The DIDP was also included among DAFNEplus assessment tools, with planned assessment of predictive validity and responsiveness to examine appropriateness of this much briefer tool for use in future interventional studies.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADDQoL-19:
-
Audit of Diabetes-Dependent Quality of Life (ADDQoL-19)
- DCP:
-
Diabetes Care Profile
- DIDP:
-
DAWN Impact of Diabetes Profile
- DSQoLS:
-
Diabetes-Specific Quality of Life Scale
- Diabetes QOL-Q:
-
Diabetes Quality of Life Questionnaire
- QOL:
-
Quality of life
References
Speight J, Holmes-Truscott E, Hendrieckx C, Skovlund S, Cooke D. Assessing the impact of diabetes on quality of life: what have the past 25 years taught us? Diabet Med. 2020;37(3):483–92.
Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome - A review of quality of life measurement in adults with diabetes. Diabet Med. 2009;26(4):315–27.
Fisher L, Tang T, Polonsky W. Assessing quality of life in diabetes: I. A practical guide to selecting the best instruments and using them wisely. Diabetes Res Clin Pract. 2017;126:278–85.
Tang TS, Yusuf FL, Polonsky WH, Fisher L. Assessing quality of life in diabetes: II–Deconstructing measures into a simple framework. Diabetes Res Clin Pract. 2017;126:286–302.
Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: a structured review. Diabet Med. 2002;19(1):1–11.
Skovlund SE, Lichtenberg TH, Hessler D, Ejskjaer N. Can the routine use of patient-reported outcome measures improve the delivery of person-centered Diabetes Care? A review of recent developments and a case study. Curr Diab Rep. 2019;19(9):84.
Holmes-Truscott E, Cooke DD, Hendrieckx C, Coates EJ, Heller SR, Speight J. A comparison of the acceptability and psychometric properties of scales assessing the impact of type 1 diabetes on quality of life—results of ‘YourSAY: quality of life’. Diabet Med. 2021;38(6):e14524.
Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27(5):1159–70.
The Food and Drug Administration (FDA). Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4(79):1–20.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, Ring L. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research practices Task Force report: part 2—assessing respondent understanding. Value Health. 2011;14(8):978–88.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, Ring L. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–77.
Rosal MC, Carbone ET, Goins KV. Use of cognitive interviewing to adapt measurement instruments for low-literate hispanics. Diabetes Educ. 2003;29(6):1006–17.
Bradley C, Speight J. Patient perceptions of diabetes and diabetes therapy: assessing quality of life. Diabetes Metab Res Rev. 2002;18(S3):S64–9.
Hilliard ME, Minard CG, Marrero DG, de Wit M, Thompson D, DuBose SN, et al. Assessing health-related quality of life in children and adolescents with diabetes: development and psychometrics of the type 1 diabetes and life (T1DAL) measures. J Pediatr Psychol. 2020;45(3):328–39.
Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999;8(1–2):79–91.
Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the diabetes care profile. Eval Health Prof. 1996;19(2):208–30.
Peyrot M, Burns KK, Davies M, Forbes A, Hermanns N, Holt R, et al. Diabetes attitudes wishes and needs 2 (DAWN2): a multinational, multi-stakeholder study of psychosocial issues in diabetes and person-centred diabetes care. Diabetes Res Clin Pract. 2013;99(2):174–84.
Holmes-Truscott E, Skovlund SE, Hendrieckx C, Pouwer F, Peyrot M, Speight J. Assessing the perceived impact of diabetes on quality of life: psychometric validation of the DAWN2 impact of Diabetes Profile in the second diabetes MILES-Australia (MILES-2) survey. Diabetes Res Clin Pract. 2019;150:253–63.
Bott U, Mühlhauser I, Overmann H, Berger M. Validation of a diabetes-specific quality-of-life scale for patients with type 1 diabetes. Diabetes Care. 1998;21(5):757–69.
Cooke D, O’Hara MC, Beinart N, Heller S, La Marca R, Byrne M, et al. Linguistic and psychometric validation of the diabetes-specific quality-of-life scale in U.K. English for adults with type 1 diabetes. Diabetes Care. 2013;36(5):1117–25.
Speight J, Woodcock A, Reaney M, Amiel S, Johnson P, Parrott N, et al. The QoL-Q diabetes’: a novel instrument to assess quality of life for adults with type 1 diabetes undergoing complex interventions including transplantation. Diabet Med. 2010;27:3–4.
Brooks J, McCluskey S, Turley E, King N. The Utility of Template Analysis in qualitative psychology research. Qualitative Res Psychol. 2015;12(2):202–22.
Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007;16(2):234–43.
Speight J, Reaney M, Barnard K. The use of hypothetical scenarios and importance weightings when measuring the impact of diabetes on quality of life. A response to Brose et al. Diabet Med. 2009;26(10):1077–9.
Lenzner T, Kaczmirek L, Lenzner A. Cognitive burden of survey questions and response times: a psycholinguistic experiment. Appl Cogn Psychol. 2010;24(7):1003–20.
Brose LS, Mitchell J, Bradley C. Comments on Speight et al.‘s ‘Not all roads lead to Rome-a review of quality of life measurement in adults with diabetes’. Diabet Med. 2009;26(10):1076–7. author reply 7–9.
Brazier J, Peasgood T, Mukuria C, Marten O, Kreimeier S, Luo N et al. The EQ Health and Wellbeing: overview of the development of a measure of health and wellbeing and key results. Value Health. 2022.
Palamenghi L, Carlucci MM, Graffigna G. Measuring the quality of Life in Diabetic patients: a scoping review. J Diabetes Res. 2020;2020:5419298.
Carr AJ, Higginson IJ. Are quality of life measures patient centred? BMJ. 2001;322(7298):1357–60.
Pickup JC, Harris A. Assessing quality of life for new diabetes treatments and technologies: a simple patient-centered score. J Diabetes Sci Technol. 2007;1(3):394–9.
Meadows K. Interpreting patient-reported outcome measures: narrative and the Fusion of Horizons. Philos Med. 2021;2(2).
Fisher L, Polonsky WH, Perez-Nieves M, Desai U, Strycker L, Hessler D. A new perspective on diabetes distress using the type 2 diabetes distress assessment system (T2-DDAS): prevalence and change over time. J Diabetes Complicat. 2022;36(8):108256.
Polonsky WH, Fisher L, Hessler D, Desai U, King SB, Perez-Nieves M. Toward a more comprehensive understanding of the emotional side of type 2 diabetes: a re-envisioning of the assessment of diabetes distress. J Diabetes Complicat. 2022;36(1):108103.
Coates E, Amiel S, Baird W, Benaissa M, Brennan A, Campbell MJ, Chadwick P, Chater T, Choudhary P, Cooke D, Cooper C. Protocol for a cluster randomised controlled trial of the DAFNEplus (Dose Adjustment For Normal Eating) intervention compared with 5x1 DAFNE: a lifelong approach to promote effective self-management in adults with type 1 diabetes. BMJ open. 2021;11(1):e040438.
Speight J, Amiel SA, Bradley C, Heller S, Oliver L, Roberts S, Rogers H, Taylor C, Thompson G. Long-term biomedical and psychosocial outcomes following DAFNE (Dose Adjustment for normal eating) structured education to promote intensive insulin therapy in adults with sub-optimally controlled type 1 diabetes. Diabetes Res Clin Pract. 2010;89(1):22–9.
Acknowledgements
We thank the adults with type 1 diabetes who participated.
Funding
This paper summarises independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme, as part of the study ‘Developing and trialling the DAFNEplus (Dose Adjustment for Normal Eating) intervention. A lifelong approach to promote effective self-management in adults with type 1 diabetes’ (Grant Reference Number RP-PG-0514-20013). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. E.H-T, C.H and J.Sp are/were supported by the core funding to the Australian Centre for Behavioural Research in Diabetes provided by the collaboration between Diabetes Victoria and Deakin University.
Author information
Authors and Affiliations
Contributions
J.Sp. and D.C. conceived the study and designed it with E.H-T., E.C. and S.H. E.H-T developed the survey and managed data collection. J.Sc. and E.H-T conducted data cleaning and analysis. All authors provided input into interpretation of results. E.H-T. and J.Sc. prepared the first draft of the manuscript. All authors contributed to manuscript revisions and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was received in Australia (Deakin University Human Research Ethics Committee: HEAG-H 03_2017) in accordance with the Australian ‘National Statement on Ethical Conduct in Human Research 2023’. Ethics approval was also received in the UK (Yorkshire & The Humber-Bradford Leeds Research Ethics Committee: 17/YH/0234; Health Research Authority: IRAS ID: 228898). Participants accessed a plain language statement and provided informed consent prior to completing the survey.
Consent for publication
Participants consented to their de-identified data being published for the current purpose.
Competing interests
Jane Speight owns the copyright for ‘Diabetes QOL-Q’. All other authors declare no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article includes data presented at a scientific meeting: Schipp J, Holmes-Truscott E, Hendrieckx C, Coates E, Heller S, Cooke D, Speight J. A qualitative investigation of the acceptability to adults with type 1 diabetes of five diabetes-specific quality of life measures. Findings of the YourSAY: Quality of Life study. Australasian Diabetes Congress (ADC) 2019, Sydney, Australia, 21-23 August 2019
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Holmes-Truscott, E., Schipp, J., Cooke, D.D. et al. Perceptions of adults with type 1 diabetes toward diabetes-specific quality of life measures: a survey-based qualitative exploration. Health Qual Life Outcomes 22, 70 (2024). https://doi.org/10.1186/s12955-024-02285-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02285-4